RECONSTRUCTIVE UROLOGY
445 East 77th Street
New York, NY 10075
(212) 241-4812

RECONSTRUCTIVE UROLOGY

445 East 77th Street
New York, NY 10075
(212) 241-4812

The channel that carries urine from the bladder to the tip of the penis is called the urethra. Urethral strictures are constrictions in the urethra caused by circular scar tissue. Which can cause a blockage in urination. This blockage can cause both “irritative” urinary problems as well as “obstructive” problems urinating. Irritative urinary problems including urinary frequency, urgency and nocturia. Obstructive problems including difficulty getting the urinary stream started – called urinary hesitancy, a slow urinary stream, and incomplete bladder emptying. Other symptoms that can occur include urinary infections and blood in the urine.
Most of these symptoms can also be caused by other problems such as an enlarged prostate in men so it can be difficult to make a definitive diagnosis based on urinary symptoms alone. If you have these symptoms an evaluation by a urologist to confirm your diagnosis might be recommended.
About 1/3 of the time urethral strictures are causes by trauma, infection, or something that causes inflammation or damage to the urethra from the patient. About 1/3 of the time strictures are caused by something doctors or nurses have done such as prior hypospadias treatment, injury from catheterization or procedures that involve inserting a scope into the urethra. The other 1/3 of the time we don’t know for sure what caused the stricture.
You might suspect a urethral stricture based on bothersome urinary symptoms. Tests that can help confirm that you actually have one include a uroflow where patients urinate into a machine that measures the speed of urination and an ultrasound measurement of residual urine. Normally, in patients who do not have a urinary obstruction, the speed of urination is fast and the bladder is emptied completely. In patients who have tight urethral strictures, the speed is slow and oftentimes urine is left behind in the bladder when checked by ultrasound. (SEE FIGURE)
Symptoms and uroflow results may increase the suspicion of a urethral stricture but these tests are not diagnostic. The two most important tests are a cystoscopy and an x-ray study called retrograde urethrogram (RUG).
Cystoscopy is a procedure where a small flexible fiberoptic scope (about the width of a pencil) is placed into the urethra to evaluate the urethra. Typically, the procedure is done in the office after the urethra is numbed up first and takes just a few minutes. It can be a little uncomfortable but rarely is it painful. On cystoscopy a normal urethra appears wide open and easily allows passage of the small scope. A urethral stricture appears as a tight narrowing in the passageway. Seeing this narrowing is diagnostic for a urethral stricture.
The problem with the cystoscopy is that your urologist cannot see behind the narrowing particularly if the stricture is very tight and symptomatic. Because of this, for most patients with tight strictures, I will also perform a retrograde urethrogram (RUG). I usually do this in the office using an X-Ray machine (called fluoroscopy) and gently inject dye into the urethra. In my opinion, it is important for the RUG to be performed by the surgeon who will potentially be treating the stricture. Small changes in patient positioning can lead to a poor quality study that may not be very accurate in giving information on the exact nature of the stricture.
In most cases, dye from the study will go through the stricture and provide information about how long the stricture is, whether a second stricture is also present and where the stricture is exactly. In my opinion it is a necessary study in patients who have tight urethral strictures.
We think it is critical to stage urethral strictures as well and have developed and validated a staging system for urethral strictures. Staging permits an assessment of the severity of the stricture, allows research to be done on strictures that permits comparisons between equivalent types of strictures, and allows doctors to communicate with each other in a more precise fashion.
The Purohit-Blaivas staging system (FIGURES) is composed of 5 stages (between 0 to 4) of strictures and is based on cystoscopic findings alone.
Stage 0: No urethral stricture is present i.e. normal urethra.
Stage 1: A urethral stricture is present but permits easy passage of a flexible cystoscope these are 16 French in size).
Stage 2: A urethral stricture is present that barely allows the cystoscope to go past it and is just the size of the scope.
Stage 3: A urethral stricture is present and does not allow passage of a cystoscope but you can still see a small hole that urine passes through.
Stage 4: A urethral stricture is present and so dense that no hole for urine is seen at all.
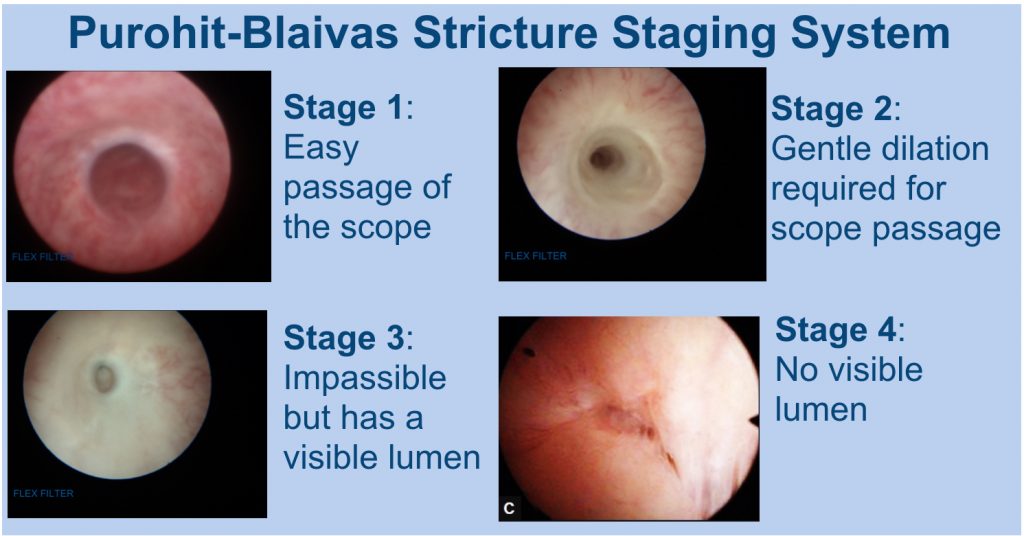
Not all strictures are the same! For example, some are wide caliber and cause no symptoms and some are very narrow caliber and cause severe symptoms. A graded system of strictures acknowledges these (though not all) differences in urethral strictures. Not all strictures need to be treated and our staging system helps clarify that. We have shown that stage 1 strictures rarely progress to more advanced stages (REFERENCE) and so are probably safe to watch. On the other hand, Stage 4 urethral strictures are usually symptomatic and generally need to be treated. The next time you hear from our doctor that you have a urethral stricture you should ask what stage it is!
Strictures are also classified as to where they are located. Anterior urethral strictures are those that are the downstream from the urethral sphincter up to the level of the tip of the penis. Posterior urethral strictures are those that involve the urethra from the start of the bladder through the prostate up to the end of the urethral sphincter.
Anterior urethral strictures can be divided further into bulbar, pendulous (or penile), fossa navicularis or meatus (tip of the penile opening) strictures. (FIGURE) Treatment options can be different for these different location strictures so location is important.
Posterior urethral strictures usually occur because of major trauma such as pelvic fractures or injury from urological procedures. The trauma can cause the urethra to get torn and as it heals it scars down become a stricture Some really bad injuries can cause the urethral to become completely disrupted from separate into 2 different parts. These strictures are often caused pelvic fracture urethral disruption defect.
There is very little data on when it is safe to watch urethral strictures. In my opinion, strictures that are stage 1, maybe stage 2 particularly if asymptomatic can probably be watched safely. Aside from causing urinary symptoms, the concern about stage 3 and stage 4 strictures being watched is that they may cause permanent damage to the bladder, urinary infections and potentially lead to acute urinary retention and the need for emergency procedure to drain your bladder.
With urethral dilation progressively larger sounds are inserted into the urethra to pop open the urethral stricture and increase the caliber of the urethral lumen. This procedure can be done in the office under local anesthesia or in the hospital under anesthesia.
Another way to do urethral dilation is to learn how to catheterize yourself to pop open the scar tissue periodically and prevent the urethral stricture from closing down.
All of these phrases are interchangeable. With a urethrotomy a cystoscope is placed into the urethra. A small blade comes out of the scope and cuts the urethral stricture from the inside to open it up. This surgery is usually done in the hospital under anesthesia but takes just a few minutes to perform. A catheter is often left in place after a urethrotomy for a few days.
This is open, reconstructive surgery on the urethra to fix the urethral stricture under general anesthesia that can be done in a variety of ways.
One way is to excise or cut out the diseased section of the urethra and put the healthy section of urethra back together. This is called an Excision and Primary Anastomotic urethroplasty or sometimes an End-to-End urethroplasty. Increasingly this surgery is being done as same day surgery and the urinary catheter is left in for about 2 weeks after surgery.
Another way to reconstruct the urethra is to use a tissue graft or flap to correct the stricture. A graft is tissue that is taken from one part of the body and implanted into another part without its blood supply still attached. A flap is the same thing but the blood supply is still attached so often it comes from tissue close to the urethra such as penile skin. In urethral reconstruction, usually the graft is taken from inside of the cheek called a buccal mucosal graft (LINK).
The nice thing about the buccal mucosal graft is that the tissue is very similar to the urethra. Like the urethra it is stretchy and suitable for a moist environment and the inner cheek and heals without too much scarring. An additional benefit is that there is plenty of it and if necessary I can use tissue from both sides of the inner cheek in long strictures. Generally, we can get about 5-7cm from each side of the mouth meaning about 10-14cm long strictures can be fixed with the BMG.
One alternative to the buccal mucosal graft is to use skin from the penis to reconstruct the urethra. If you think about it, the skin on the shaft of the penis is stretchy, in uncircumcised men the foreskin is abundant and can also be used. Long strictures can be repaired with a local skin flap. If possible, I generally prefer the buccal graft and save the flaps for when a BMG is not possible.
Data has shown that urethral dilations and urethrotomy have equivalent outcomes. Both are fairly easy to do as outpatient surgeries. In most patients, however, there is a very high rate of recurrence of the stricture. In fact, after one failed urethral dilation or urethrotomy the long term success of a second dilation or urethrotomy is close to 0 (zero!) percent, or put another way, everyone will have a recurrent stricture. The best patients for these procedures are those who are too sick to have a urethroplasty, have very filmy strictures and have not had prior urethral dilations or urethrotomy done before.
The reason stricture can have such a high recurrence rate is that most anterior strictures are accompanied by underlying disease in the spongy tissue that is deep to the lining of the urethra. The anterior urethra is like a long tubular donut with urine flowing through the hole of the donut. A stricture is when the hole of the donut narrows and become constricting. However, the real problem with most urethral strictures is that the spongy part of the donut, called the spongiosus, has scar tissue that develops in it. This scar tissue is called spongiofibrosis (FIGURE).
If you have a urethrotomy or urethral dilation this underlying problem of spongiofibrosis is not corrected and causes the stricture to return. In fact, some data has suggested that every time you have a urethrotomy or dilation done, the cutting of the tissue can cause more scar tissue to form in the spongiosus and extend the spongiofibrosis further. This can make a simple urethral stricture more complex making repair of the stricture more difficult in the future.
With this surgery, all of the spongiofibrosis is being excised so, essentially, I am aiming to cure the underlying problem. Consequently, the success rates are fairly high for this type of urethroplasty with most data suggesting over an 90% long term success rate or put another way, just a 10% failure rate. In the 10% of patients for whom the stricture does recur, it can still be repaired with either a dilation, urethrotomy or another urethroplasty. The EPA urethroplasty does have some limitations and problems, however. For one, it can only be used on shorter strictures less than about 3 cm in the bulbar urethra. If the stricture is longer or towards the tip of the penis, excising that section of the urethra can distort the penis causing it to curve downwards, particularly with erections, in a condition called chordee. There is a small chance of developing worsened erections (estimated to be about 1-5%) after surgery. More recently, some reconstructive urologists have raised concerns about transecting the urethra because doing so might compromise the blood supply to the urethra downstream from the urethroplasty. On this the jury is still out!
One of the advantages of the BMG urethroplasty is that it can be used for longer strictures in the any part of the anterior urethra. I have successfully repaired strictures that started all the way from the sphincter to the tip of the penis using only buccal grafts. This type of the urethroplasty also has a lower risk of erectile dysfunction than the EPA urethroplasty (<1%). Its success rates are not as high as EPA urethroplasty and are probably around 80% at 10 year. However, the longer patients are followed, the lower the success rates are for this type of surgery. But most of the time that we are repairing these in very long complicated strictures so this rate is acceptable to most patients as they have often failed multiplied prior dilations or urethrotomies.
Posterior strictures are strictures that occur anywhere from the neck of the bladder down to the level of the level of the sphincter. These are different from anterior strictures because in this area there is no urethral spongiosus present so there is no accompanying spongiofibrosis. Most of the time these strictures are caused by external trauma or abnormal healing from surgical procedures.
For strictures that are closed to the sphincter from pelvic fractures there is dense scar tissue between the urethra and the prostate. This scar tissue has to be cut out surgically and the two healthy ends of the urethra are put back together. For strictures at the level of the bladder neck called bladder neck contractures these are usually repaired robotically by placing small ½ inch incisions on the abdomen and placing small robotic instruments to correct the problem.
YES! He accepts all major insurances including Medicaid and Medicare.
As the Director of Reconstructive Urology at Mount Sinai, Dr. Purohit is often referred the most complicated cases that other urologists find difficult to treat. He has treated approximately 1000 patients with urethral strictures.
EXCELLENT! There are no guarantees but his results compare favorably with anyone in the world. You can see some of his before and after urethroplasty photos best illustrated with the retrograde urethrogram.